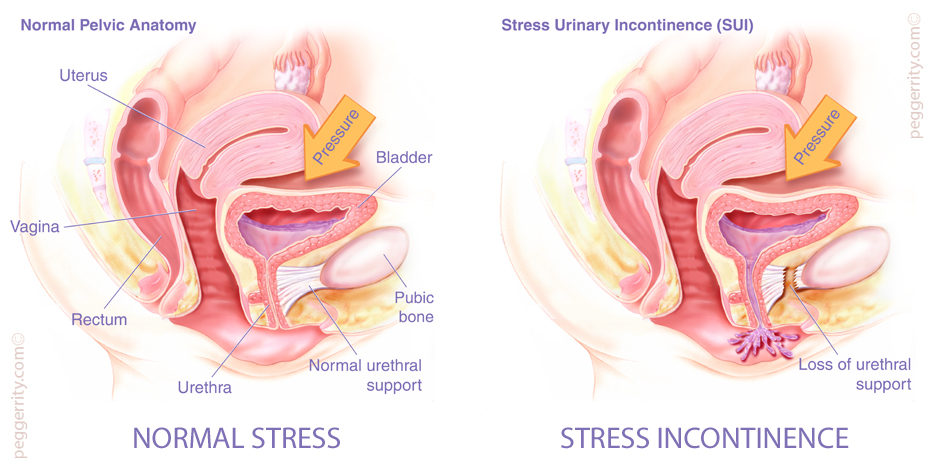
Stress incontinence, is by far, the most common type of incontinence which accounts for about 75% of cases seen by physicians and can occur in any stage throughout a women’s life: high school, college, pregnancy, following childbirth, and on into menopause. It is a loss of urine that happens during exercise, coughing, sneezing, laughing, lifting heavy objects, or other body movements that put pressure on the bladder. Most of the time, this condition results from weakening of the pelvic supportive structures for the bladder, bladder neck, and urethra that can occur due to pregnancy, childbirth, obesity, lack of hormonal support, and prior pelvic surgery.
TREATMENT
Treatment for Stress Incontinence depends greatly on an individual’s capabilities and desires.
Behavioral Therapy
Behavioral Therapy is to help train women to behaviorally control mild to moderate incontinence. For example, certain foods and beverages contribute to urgency or increased frequency (i.e., urge incontinence). Therefore, many women find that reducing or eliminating their caffeine intake lessens these symptoms. Also, timed voiding and bladder retraining, which involve urinating on a set schedule during the day regardless of the need or urge to void, is often helpful.
Pelvic Muscle Exercises
Pelvic Muscle Exercises (sometimes called “Kegel exercises”) can be helpful for mild stress or urge incontinence. When properly and consistently performed these exercises can strengthen the sphincter muscles and lessen the degree of incontinence.
Biofeedback
Exercise and behavioral training can both be enhanced by biofeedback and thereby help women with urinary incontinence. During biofeedback training, a probe inserted into the patient’s vagina sends images to a television monitor, which allows patients to watch the muscles’ response as they are squeezed. The monitor helps women know when they are contracting the proper muscles, and it guides the training sessions toward better muscle endurance.
Medications
Medications used for stress incontinence work by enhancing urethral closure pressure. Although there are drugs available that can be used to minimize this condition, they will rarely be curative. The first class of drugs is the alpha-agonists which act to increase the tone of the urethra and bladder neck, thereby increasing the outlet resistance of the bladder. Women with mild to moderate stress incontinence will generally get more relief than those women with severe incontinence. The main side effect of the alpha-agonists is hypertension which limits their usefulness in the older patient.
Estrogens have been shown to be helpful in urinary incontinence. Postmenopausal women develop urogenital atrophy, a thinning of the tissues, which can impair the urethra’s ability to close and result in irritative symptoms such as urgency, dysuria and overactive bladder. Estrogen helps restore this urogenital lining and desensitizes the bladder, thus helping both stress and urge incontinence. Though all forms of estrogen can alleviate these symptoms, local administration through the use of vaginal estrogen cream or tablets provides the most rapid response.
One of the newer drugs available specifically for the treatment of stress incontinence is duloxetine, a selective inhibitor of serotonin and norepinephrine reuptake. By blocking the reuptake of serotonin and norepinephrine in the spinal cord, duloxetine is thought to increase contraction of the urethral sphincter.
Medical Devices
Medical Devices are for women who do not experience relief with non-surgical treatments but do not yet wish to undergo surgery. Options available are urethral plugs and patches, vaginal tampons, pessaries (diaphragm-like devices that support the vagina), catheters, pelvic organ support devices, external collection systems, and absorbent products.
Surgery
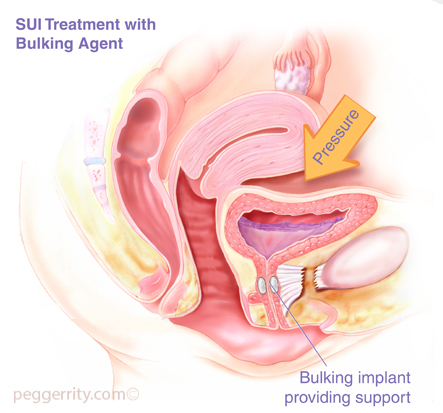
There are many different surgical procedures that may be used to treat incontinence. The type of operation recommended depends on the type and cause of the incontinence. Some of the more common procedures performed are bladder neck suspension or sling procedures, periurethral bulking injections (collagen injections around the urethra), restoration of the normal support of the pelvic floor, implantation of an artificial urinary sphincter or sacral nerve stimulator.
The mainstay of treatment for significant stress urinary incontinence is surgery. In the past it was felt that most stress incontinence resulted from two distinct scenarios:
- Urethral Hypermobility in which there was an unequal pressure-transmission ratio to the bladder and proximal urethra
- Intrinsic Sphincter Deficiency (ISD)
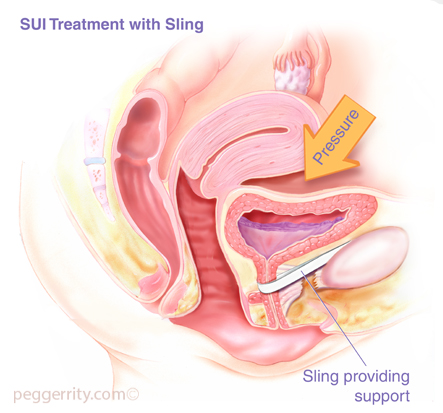
SUI Treatment with Sling
Different surgeries were used to address each of these situations. For urethral hypermobility it was felt that a retropubic urethropexy would “re-establish” normal anatomy thus resulting in continence. In patients with intrinsic sphincter deficiency, a “sling” was use to provide added support to the deficient sphincter, and sometime obstruction. Recently the distinction between the two scenarios has become blurred and it is felt by many that intrinsic sphincter deficiency exists along a spectrum rather than being an “all or nothing” phenomenon. And as such, it is felt that all patients with stress urinary incontinence suffer from some degree of ISD. In accordance with this thinking and the development in the tension-free mid-urethral tape procedures over the last several years, slings have taken the forefront as the first-line surgical correction of stress urinary incontinence.